Treatments
Surgeries
Most shoulder surgeries can be performed on an outpatient basis whereby the patient can go home the same day.
Arthroscopic surgery is performed with a pencil-sized camera and several half inch incisions to repair the torn tissue, remove bone spurs, and clean out inflamed tissue.
Open surgery is performed through a 3-5 inch incision over the front or top of the shoulder and is used for shoulder replacements, shoulder stabilizations, and acromio-clavicular joint debridements.
Below is a brief synopsis of many surgeries that are offered. Although the procedures are listed individually, it is more common that multiple procedures are combined during someone’s surgery. For example, a patient may have a subacromial decompression, a rotator cuff repair and a biceps tenodesis all at the same setting. The rehabilitation for these multiple procedure surgeries follows the rehabilitation for the biggest surgery (in this case, it would follow the rehabilitation for the rotator cuff repair). In general, physical therapy lasts until the patient has pain-free full range of motion. Strengthening is commenced at therapy but often continues after the patient has been discharged to a home exercise program, which typically occurs 3-6 months after surgery.
All surgeries have a risk and reward associated with them. Pain relief is the reward but the risks include infection (occurs 1% of the time), stiffness (occurs in many patients and is the cause for the need for physical therapy), and persistent pain (the majority of surgeries have a 80-85% chance of success and a 15-20% chance of persistent pain). Because of the downsides to surgery, all patients are encouraged to cure their pain with non-operative means first. Although surgery is no guarantee for success, the odds of people getting worse with surgery are less than 5%. For that reason, surgery can be an attractive option for people with chronic, intractable pain.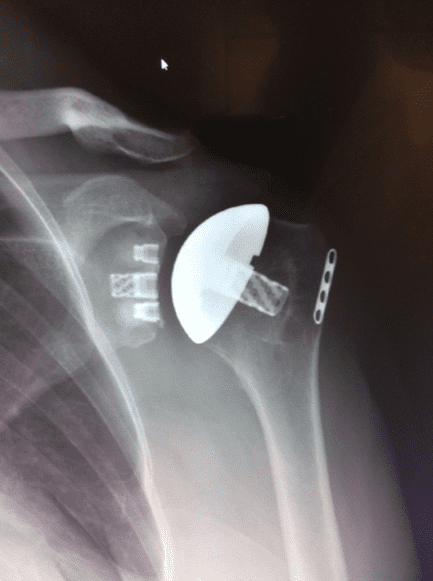
AC Joint Reconstruction
A shoulder separation is a tear of the Acromio-Clavicular (AC) joint ligaments. When the tear is significant enough to also involve the Coraco-Clavicular (CC) ligaments, the AC joint can become unstable and necessitate surgery.
Surgery is performed on an outpatient basis through a small open incision. The AC and CC ligaments are reconstructed with either a polyester tape or a tendon. Patients stay in a sling for 2-4 weeks and can return to normal activities by 6-8 weeks and contact sports at 12 weeks.
Arthroscopic Debridement and Capsular Release
This procedure is performed for people with pain emanating from their shoulder (glenohumeral joints). Two common causes for pain include arthritis and adhesive capsulitis (also known as frozen shoulder).
Loose bodies are common in arthritis and can be washed out quickly with the arthroscope. Tight ligaments can be released in a frozen shoulder.
This procedure, which takes thirty minutes to perform, is an outpatient surgery. Patients are home within a few hours of the procedure and usually wear a sling for a day or two only. Physical therapy is started on post-operative day #1 to maintain the range of motion obtained at the time of surgery.
Click here to view a video on Capsular Release.
Click here to view a video on Loose bodies.
Bankart Repair, Labral Repair, the Latarjet Procedure and Instability Surgery
Ligaments connect the humerus and the glenoid together. A frozen shoulder (adhesive capsulitis) occurs when the ligaments are too tight. A loose shoulder occurs when the ligaments are too lax. Because the ligaments attach to a rim of cartilage surrounding the socket called the labrum, a labral tear (when the labrum is detached off the socket) causes instability. Labral tears that occur in the bottom part of the socket (glenoid) can cause the shoulder to dislocate. When this problem is not remedied with therapy, arthroscopic surgery is very effective in stabilizing the shoulder more than 90% of the time.
A SLAP tear occurs when the labrum is detached off the top of the glenoid, especially when it involves the insertion of the biceps tendon. SLAP is an acronym for Superior Labral Anterior to Posterior. It refers to labral tears that occur on the top of the socket that extend from the front of the socket to the back. Often, these tears cause pain deep in the shoulder with throwing motions and can be fixed arthroscopically.
Typically performed in an hour, these surgeries allow the patients to go home the same day as the surgery. Patients are kept in a sling, especially at night when they sleep, for the first 3-4 weeks. Therapy is initiated within a week after surgery and is needed for 3-4 months.
The Latarjet procedure is performed by transferring the coracoids and its attached muscles to the front edge of the glenoid where it is fixed with screws. This builds up the diameter of the shoulder socket and increases the stability of the joint. The Latarjet procedure is performed in cases of recurrent instability and those with bone loss.
Visit our YouTube channel for a specific video on this topic.
The biceps tendon runs up the front of the arm and has two attachment sites. The short head inserts onto the coracoid process and the long head inserts onto the top of the glenoid where it blends into the labrum. When the long head of the biceps is torn or inflamed, it can be a source of pain that radiates down the front of the arm. Cortisone injections can be very effective in treating this pain but sometimes surgery is needed. During a biceps tenodesis, it is preferred to remove the long head from its attachment onto the top of the socket and re-attach it to the humerus. See pictorial (PDF).
This procedure takes twenty minutes and afterwards the patient is kept in a sling for a few weeks and asked not to actively flex their biceps in order to protect the repair site. This procedure is very effective in eliminating any pain originating from the long head and is often combined with other procedures about the shoulder.
Bursectomy and Acromioplasty aka Subacromial Decompression
Performed arthroscopically, this procedure removes the inflamed bursa that accumulates under the acromion and on top of the supraspinatus (one of the four rotator cuff muscles). The acromion is inspected, too, and often has a bone spur or hook that impinges on the bursa and supraspinatus tendon. If a bone spur is found, it is removed at the same time.
This is the most common procedure performed and alleviates the pain on the top and side of the shoulder that occurs when people reach overhead, reach behind (as in putting on a coat), or sleep on the affected shoulder. When the patient has arthritis and pain coming from the acromioclavicular joint (AC joint), we excise the end of the clavicle (the distal aspect of the clavicle) at the same time.
Performed on an outpatient basis, this procedure takes twenty minutes (thirty if the distal clavicle is excised). Postoperatively, the patient is in a sling for 3-5 days and starts physical therapy within a week.
Visit our YouTube channel for a specific video on this topic.
Although just about everyone over the age of 30 has x-ray findings of arthrosis of the acromio-clavicular joint, only some people have pain coming from that joint. When non operative treatment fails (observation, anti-inflammatories, creams, injections), surgery is considered. Excising the end of the clavicle is the treatment for symptomatic arthritic acromio-clavicular joints. This surgery can be done arthroscopically or through an open techque. Many have found, ironically, that the open technique has a quicker recovery.
Click here to view a video on Distal Clavicle Excision.
Fracture Fixation
Fractures are very common about the shoulder, with clavicle fractures one of the most commonly fractured bones in the body. Most clavicle fractures are treated non-operatively and will heal in the same manner as rib fractures. Sometimes, the clavicle breaks with such a tremendous force that the fragments are widely separated.
In this scenario, it is unlikely the fragments will knit together and surgery is needed. Plates and screws are the preferred method to connect the bones.
Fractures of the top of the humerus also can be displaced or non displaced. Again, the use of plates and screws is the preferred fixation technique to maximize the chance of getting the bones to heal in an anatomic fashion. When the bone is shattered into several fragments, it may not be possible to piece everything back together perfectly. In this situation, it is preferable to perform a partial shoulder replacement.
The risks of surgery to fix fractures about the shoulder include those listed above as well as risks that occur in any fracture surgery about the shoulder. These include nerve damage, which can present as numbness, just beneath the clavicle after fixation of clavicle fractures. Another risk is a nonunion, which occurs when the bones refuse to heal. Despite putting the bones together with plates and screws, the surgery does not heal the bone. Time heals the bones together. Smokers are more prone to nonunions, which need more invasive surgery to fix.
Visit our YouTube channel for a specific video on this topic.
There are four rotator cuff muscles that originate off of the scapula. Their respective tendons form a cuff of tissue that inserts onto the top of the humerus. Each tendon rotates the humerus.
When one of these tendons tears off the humerus it is called a rotator cuff tear.
The tear alters the mechanics of the shoulder and causes pain and limitations in function. If the tear is big enough, physical therapy will not help alleviate the pain. In this situation, surgery is indicated to repair the torn tendon back to the bone. This surgery is performed arthroscopically, which offers less pain than an open rotator cuff repair.
The surgery is performed on an outpatient basis and typically takes 45 minutes to perform. Sometimes more than one tendon is torn off the humerus and multiple tendons have to be repaired. To prevent the repaired tendon from detaching, the arm is kept in a sling for 3-8 weeks, depending on the size of the tear. During this period, the patient goes to physical therapy for manual therapy to prevent a stiff shoulder. Therapy is usually needed for 4-6 months after surgery. The success rate of shoulder surgery is dependent on several factors, including the number of tendons torn (more is bad), the time from tear to surgery (the sooner surgery is performed the better), and patient factors (smoking is bad). Most healthy people with small to medium tears can expect a 90% success rate from this surgery.
Visit our YouTube channel for a specific video on this topic.
Shoulder Replacement Surgery
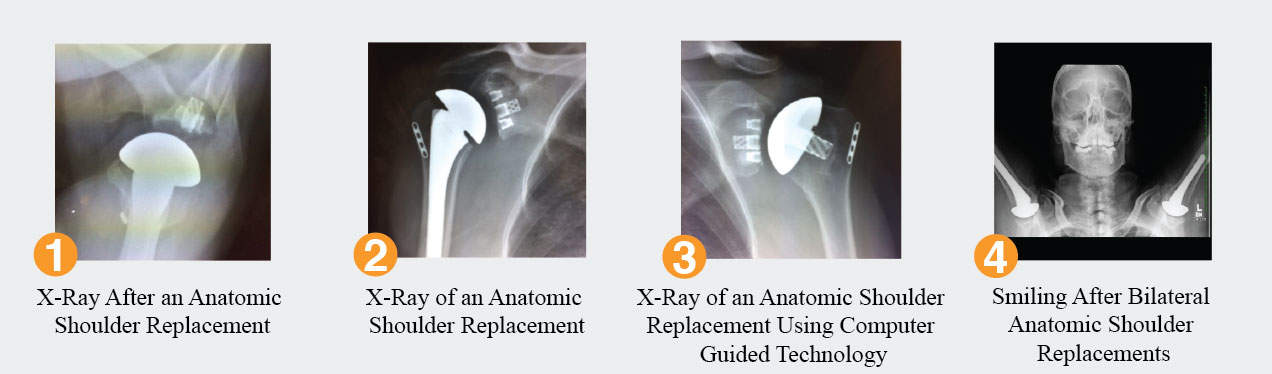
What’s New in Shoulder Replacement Surgery
Although much improvement has been made in the realm of shoulder replacement surgery over the last 30 years that has led to results similar to hip and knee replacements, there continues to be a push towards less invasive surgery with quicker recoveries and longer lasting excellent results.
Advances in anesthesia and smaller incisions have made it routine for shoulder replacement surgery to be performed on an outpatient basis where the patient goes home on the same day as surgery. Many patients prefer to recover and sleep in their own home, eating their own food, and being cared for by family members instead of nurses. A few hours after surgery, patients are able to eat solids and walk on their own. Family members are needed for the first 1-2 days to assist the patient in getting out of a chair, with dressing, and with food preparation.
Advances are also being made with the technology being used by surgeons. Computer navigation and GPS allows the surgeon to place the components more accurately with less need for bone resection. Although it will take years to see if these new techniques improve upon our current results, surgeons and engineers believe that more accurate positioning of the polyethylene and metal components combined with less bone resection will lead to even better results and longevity.
Shoulder Replacement Surgery: Total Shoulder Arthroplasty and Reverse Shoulder Arthroplasty
When arthritis affects the glenohumeral (ball and socket) joint, attempts are made to treat the pain non-operatively with a combination of medications, physical therapy and activity modification. When these modalities fail to relieve the pain, a shoulder replacement is performed. These are open procedures performed through a minimally-invasive approach. Fifty percent of patients go home the same day. Those patients who live alone often need to stay two nights. A sling may be worn for three weeks after surgery and physical therapy typically lasts three months.
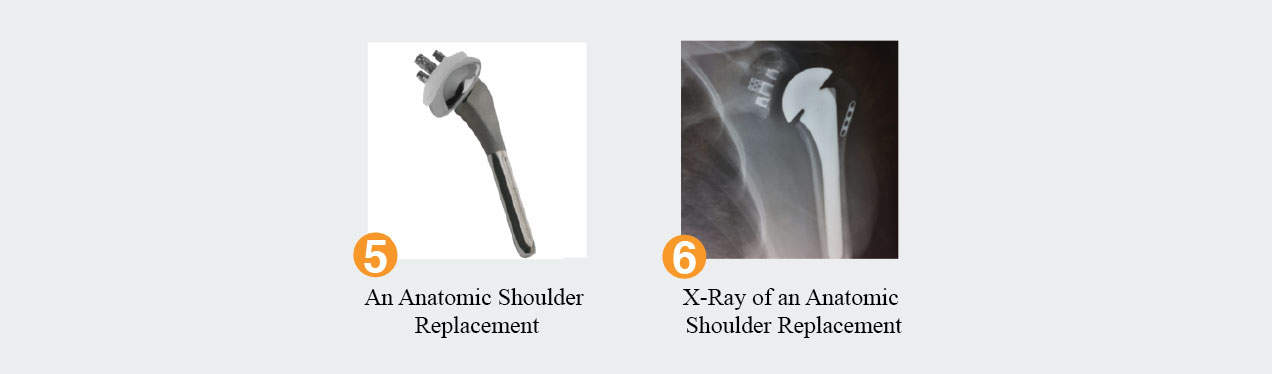
A routine total shoulder replacement is performed when the rotator cuff muscles are intact. Designed to take away the pain from bone on bone arthritis, the procedure replaces the humeral head with a chrome ball attached to a titanium stem in the humerus. The glenoid is replaced with a polyethylene (medically grade plastic) socket. Cement is rarely needed on the humeral side but is always needed on the socket side. Pain relief and improved function is seen in 90% of patients who undergo this procedure, which is an excellent option to treat advanced arthritis of the shoulder joint.
A reverse shoulder replacement is used to treat arthritis in the setting of a torn or nonfunctioning rotator cuff. The rotator cuff tendons normally counteract the superior pull on the arm that the deltoid muscle provides. The rotator cuff tendons keep the humeral head centered on the glenoid socket. When the rotator cuff tendons are no longer working, the humeral head migrates superiorly because of the unopposed pull of the deltoid. The reverse shoulder replacement pushes the humerus down and puts the deltoid under tension.
The downsides of shoulder replacements are the same for all surgeries (infection, stiffness, persistent pain) with two new caveats. One is the fact that these artificial joints do not last forever. Patients are encouraged to avoid significant weight bearing with their new shoulder (avoid weight lifting and rock climbing) to make the components last. The other injury germane to any open surgery about the shoulder joint is injury to the nerves around the shoulder. Rarely injured during surgery, nerves are more at risk during revision surgery because they are encased in scar tissue that may need to be dissected. Nerve damage can present as muscle weakness and may take several weeks or months to improve.
An unusual source of pain is the joint between the shoulder blade and the ribs. A film of bursa provides lubrication between these two surfaces and can become inflamed and thickened. Presenting as a crunching that emanates from the top of the shoulder blade, this bursitis can be especially painful for some patients.
When therapy and cortisone prove unsuccessful, a surgical procedure whereby the top corner of the scapula and bursa are excised is considered. Patients usually spend one night in the hospital and wear a sling for 4 to 6 weeks after surgery to allow the muscles to heal properly.
Subcoracoid Decompression
Similar in nature to the subacromial decompression, this procedure is performed when the coracoid impinges on the subscapularis (one of the four rotator cuff muscles). A common cause of pain in the front of the shoulder with shoulder motion, this procedure takes minutes to do and has practically no need for a sling post-operatively.
Visit our YouTube channel for a specific video on this topic.
Non-Operative Treatment
Most conditions about the shoulder can be treated non-operatively. Only a few conditions, such as rotator cuff tears and fractures, will lead to disabling, painful arthritis. The remaining conditions about the shoulder will not lead to arthritis and patients are often encouraged to treat their pain with simple modalities such as rest and non-steroidal anti-inflammatory medications such as naproxen or ibuprofen. When the pain persists longer than three or four weeks, patients may be offered cortisone injections, physical therapy, or other pain relieving modalities.
Physical Therapy
Philosophy on Physical Therapy
The key to a happy shoulder is a flexible shoulder. Initial phases of physical therapy should focus on decreasing the inflammation about the shoulder with anti-inflammatory medications and ice. Once the inflammatory phase of healing has passed, the next phase is to restore range of motion.
Since a stiff shoulder is a painful shoulder, restoring the range of motion is the most important part of rehabilitating the shoulder. The stiffness usually manifests itself in the glenohumeral joint. The glenohumeral stiffness is first seen in the anterosuperior aspect of the shoulder joint in the area known as the rotator cuff interval. This causes a limitation with external rotation or reaching behind. As the stiffness progresses the inferior and posterior aspect the shoulder joint get stiff. This causes difficulty with overhead and behind-the-back reaching.
In the case of adhesive capsulitis (frozen shoulder), the only effective way to maximize the range of motion of the stiff glenohumeral joint is manual therapy. This mandates that a therapist stabilizes the scapula and mobilizes the glenohumeral joint. Without manual stabilization of the scapula, as seen in patient directed exercises, the scapula will move on the ribs and this scapulothoracic motion will substitute for glenohumeral range of motion. Self directed and pulley exercises will not be of much benefit in stretching out a stiff (glenohumeral joint) shoulder because the scapula will hike up. Someone (a therapist) needs to keep the scapula in place while stretching out the stiff ball and socket (glenohumeral) joint.
The final stage of therapy is strengthening. Once the glenohumeral range of motion is optimized, the periscapular muscles must be strenghthened to address the various problems around the shoulder. People with bursitis, impingement or rotator cuff tendinitis usually have good range of motion and their therapy can start at this stage. Rotator cuff weakness can cause subtle instability and pain in the overhead athlete and needs to be addressed. Impingement syndrome can be addressed by strengthening the scapular stabilizers such as the serratus anterior, rhomboids, and lower aspect of the trapezius. These muscles help elevate the anterior acromion and maximize the acromiohumeral distance which minimizes impingement.
Biologics
A new and exciting evolution in the treatment of musculoskeletal ailments is the use of biologic solutions. Historically, orthopaedic research has been focused on making the strongest implants whether they are joint replacements, plates and screws to fix fractures, or suture material to repair torn tendons. It has become quite evident over the years that the implants available to physicians are more than strong enough to withstand the forces applied by our bodies during our active lifestyles. The weak link in healing the damaged tissue is the biology of the tissue. If we use the strongest suture to tie a tendon to the bone and the tendon has the consistency of Jello, the tendon will simply pull out of the tendon. More and more research is being directed to improve the biologic characteristics of our tissue to improve healing and PRP injections and stem cells from bone marrow and fat tissue are an early venture into this arena.
Patients who receive PRP injections have two tablespoons of blood removed in the office setting and the blood is then put into a centrifuge. The centrifuge separates the blood into two components. The heavy cellular component comprised of red and white cells sinks to the bottom of the test tube and the golden plasma floats above. The cellular component contains the inflammatory mediators that our bodies use to attack infections and stimulate an eventual healing process. The plasma contains platelets that is rich in growth factors that can directly stimulate a healing process. Essentially, PRP may be considered a way to convert an inflammatory process to a healing process.
Although used for years in other fields of medicine, PRP injections are new to orthopaedics and research studies on their efficacy are currently being undertaken. Without a doubt, their use will be perfected and they will be shown to decrease the healing time of various soft tissue ailments. Although these injections can not be expected to cure structural problems such as tendon tears or cartilage loss as seen in arthritis, they can expedite the healing of partial tendon and ligament tears (hamstring tears, tennis elbow, rotator cuff tendinosis).
There is hope that we can use a patient’s own tissue to heal cases of tendintis and mitigate the symptoms of arthritis. Stem cells are another exciting area in orthopaedic research. These cells can be harvested from bone marrow (pelvis) or subcutaneous fat. Compared to the growth factors seen in PRP, these stem cells are thought to create a more powerful healing response. The stem cells are pluripotential cells meaning that, when placed in an osseous environment, they have the potential to form bone and, when placed in a cartilage environment, they have the potential to form cartilage. They also have the potential to form tendon cells when placed in tendons and muscle cells when placed in a muscular environment.
As with any nascent technology, the literature on biologics will explode in the next several years and one should consult their own physician for the latest update on this topic. Personally, I think it is a very exciting advancement in the treatment of musculoskeletal disorders, one where we are using a patient’s own tissue to facilitate the healing process.
Cortisone
Facts About Cortisone
A common question asked is about the safety and efficacy of cortisone. Cortisone is one of the best treatments in my arsenal, yet, people continually ask one of three queries: “Doesn’t cortisone damage the tissue?”, “Doesn’t cortisone mask the pain so that I can do more damage?”, and “Isn’t cortisone only temporary?” The answer to all three questions is no. Frequently theses misperceptions are spawned by family or friends who have heard little tid-bits of information.
“Doesn’t cortisone damage the tissue?”
Before I answer “No”, one has to understand that too much of anything is not healthy. Eating a bottle of Tylenol will destroy your liver and possibly worse, but we all know that Tylenol is as safe a drug as there is. The same holds with cortisone. Massive amounts of cortisone do weaken the collagen in ligaments, but the amounts used by doctors have no deleterious effects. So a small amount of cortisone once in a while is perfectly safe. Still, because of the potential effects on collagen, most doctors have a “three strikes and you’re out” philosophy. If the third injection of cortisone has not cured the problem, the fourth probably won’t and it is better to seek alternative treatments.
“Doesn’t cortisone mask the pain so that I can do more damage?”
No, no, no. Novocain (lidocaine or marcaine) can mask the pain but not cortisone. Media reports stated that Curt Schilling received marcaine shots in his ankle in 2004 (the year of the bloody sock) before he pitched. Those shots numbed the ankle so he could not feel the pain and more damage could have occurred. But cortisone does not mask the pain; it fixes the pain by decreasing the inflammation, which is causing the pain.
“Isn’t cortisone only temporary?”
Sometimes, but often it is permanent! Cortisone is a potent anti-inflammatory, like a strong Advil or Motrin or Aleve. Cortisone decreases the inflammation and the pain that accompanies the inflammation. Unlike Novocain, cortisone fixes the problem. If the cause of the inflammation persists, the inflammation and pain can return. For instance, cortisone will decrease shoulder pain from rotator cuff impingement or bursitis. But, if the patient returns to a lot of overhead activities (for instance painting ceilings or swimming freestyle), the inflammation will return as will the pain.
I hope this helps set the record straight. I know there is a fourth question on many people’s minds, “Don’t cortisone injections hurt?” Well, to be truthful, I wouldn’t want one every day of my life, but the shoulder has fewer nerve fibers than other parts of the body, so many cortisone injections around the shoulder are well tolerated.
Diagnosis Tool
Use this as a guide to determine what could be wrong based on the symptoms exhibited. For example, if your symptom is mild pain, then the most likely diagnosis could be one of the following: 1. Impingement, 2. AC Joint Arthritis, or 5. Superior Laberal Tear (SLAP Tear).
Diagnosis
Impingement
AC Joint Arthritis
Glenohumeral Arthritis
Frozen Shoulder
Superior Labral Tear (SLAP Tear)
Anterior Labral Tear
Rotator Cuff Tear
Rotator Cuff Arthropathy
Calcific Tendinitis
Tumor
Disclaimer: By no means does this experimental diagnosis tool substitute for a physician’s opinion. It has NOT been validated as an accurate diagnosis maker and is only supplied for educational purposes to give a patient an idea of what symptoms could correspond to what diagnoses. It is strongly recommended that you seek formal medical advice from your physician instead of relying on this tool.